Cooled Versus Conventional Thermal Radiofrequency Neurotomy for the Treatment of Lumbar Facet Pain
Point/Counterpoint
Guest Discussants: Prempreet S Bajaj, DO, Jonathan Napolitano, MD, Wenbao Wang, MD, Jianguo Cheng, MD, PhD
Feature Editor: Jaspal Ricky Singh, MD
Lumbar facet pain is a specific type of lower-back pain.
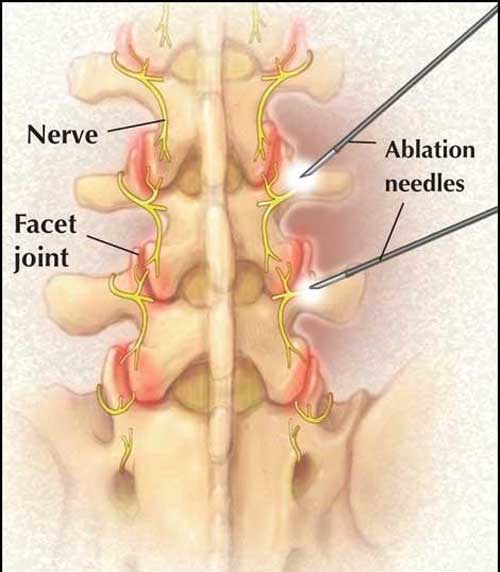
Facet joints are located at the top of the cervical spine in the neck all the way down to the lumbar spine in the lower back; they keep the spinal vertebrae aligned. Each facet joint has 2 small spinal nerve branches called medial nerves.
What causes lumbar facet pain?
Besides injury or accident, the most common cause of lumbar facet pain (or lumbar facet-mediated pain) is the degeneration or arthritis of the facet joints.
Lumbar facet pain is often confined to the lower back, but can travel into the buttock and down the back of the thigh. It rarely travels below the knee, as does pain from a herniated disc. Most people with facet-mediated back pain typically experience lower back pain that becomes worse with twisting, standing, or bending backward. This condition is common among older adults.
How is lumbar facet pain treated?
There are several options for treating the pain and symptoms caused by facet arthropathy:
- Oral anti-inflammatory medications to help reduce pain and inflammation.
- Physical therapy to help improve the strength and endurance of the muscles in the lumbar spine.
- Epidural steroid injections (ESIs) to help relieve some of the pain and discomfort of facet arthropathy by reducing inflammation. Read more about ESIs.
- Medial branch (nerve) blocks to confirm suspected facet pain. An anesthetic is injected near the small medial nerves connected to the facet joint. If pain relief is experienced immediately after the injection, then the facet joint is determined to be the source of the patient’s pain. It provides only short-term relief.
- Radiofrequency neurotomy (RFN)—also called radiofrequency ablation—is a minimally invasive procedure in which a thermal lesion (burn area) is created on the irritated nerve tissue. The radiofrequency currents are applied through an electrode placed near the target nerve to interrupt the pain signal to the brain.
- With conventional RFN, radiofrequency currents generate heat (80-90°C) around the nerve to create the lesion.
- With cooled RFN, water-cooled radiofrequency (60°C) is used to create the lesion.
- Surgery may be necessary when there is nerve root compression from disorders of the lumbar spine such as degenerative disc disease, spinal instability, or spinal stenosis.
In the October 2015 issue of Pain Management & Rehabilitation Journal, four physicians shared differing opinions about treating lumbar facet pain. A patient’s case is presented here, followed by a debate as to the best treatment plan. Drs Prempreet Bajaj and Jonathan Napolitano advocate for cooled RFN, arguing that this procedure is safe and results in improved patient outcomes. Drs Wenbao Wang and Jianguo Cheng argue that evidence of the benefits of cooled RFN is limited and that the increased costs do not justify its use.
Patient case
Selena, a 59-year-old woman, comes into the spine clinic with low-back pain on her right side. She has been experiencing this pain off and on for the last several years with no history of trauma or injury. The pain gets worse when Selena is standing in place but improves when she is walking or sitting. The pain is confined to her right, low back, and buttock regions.
Selena is given a physical examination; her sensory, motor, and muscle stretch reflexes are all normal. Selena experiences pain when she extends or twists her spine, which indicates the lumbar spine is the source of her symptoms. Magnetic resonance imaging (MRI) of the lumbar spine reveals mild disk degeneration and evidence of facet joint arthropathy.
Selena is diagnosed with lumbar facet-mediated pain and receives diagnostic medial branch blocks. After positive responses (greater than 80% reduction in pain) to 2 sets of medial branch blocks, she returns to the spine clinic to discuss the next steps. Selena recently saw an advertisement for cooled radiofrequency neurotomy (RFN) and would like to consider this option.
Prempreet S Bajaj, DO, and Jonathan Napolitano, MD, respond
Selena’s case is a very common scenario that is seen widely throughout pain practices in the United States. Many patients, including Selena, often present with chronic low-back pain, likely originating from spine degeneration or arthritis in the lumbar facet joints.
Lumbar facet pain most commonly affects the lower back and buttocks; less commonly affects the thigh, hip, and groin; and rarely travels below the knee. Selena’s diagnosis is made based on clinical history, physical examination findings, and imaging of the facet joints.
However, the most valuable and reliable tool is the medial nerve branch block: a procedure in which an anesthetic is injected near the small medial nerves connected to a specific facet joint. The 2 separate diagnostic blocks, which provided pain relief greater than 80%, confirm Selena’s facet arthropathy diagnosis.
Typically, a patient with facet arthropathy that is confirmed by medial nerve branch blocks is a good candidate for radiofrequency neurotomy (RFN), assuming other treatments, such as physical therapy and anti-inflammatory medications, have not been successful.
For many years pain physicians have used conventional RFN to reduce pain from facet joints. However, understanding the limitations of conventional RFN explains why cooled RFN is a more attractive pain management tool.
Typically, patients with chronic low-back pain from facet arthropathy also have significant degeneration of the spine, with osteophytes (bone spurs) and calcium buildup that makes it difficult place the needle correctly.
Why is cooled RFN preferable?
Using a water cooling system, cooled RFN was initially developed for various applications in cardiology and oncology. It creates a lesion twice the size of that in conventional RFN. Also, a conventional RFN lesion is elliptical in shape, requiring the probe be placed parallel to the nerve, while the cooled RFN needle can be placed perpendicular to the nerve because the burn area is a sphere.
Cooled RFN is preferable because it:
- Is a more efficient, faster procedure
- Creates a sphere-shaped lesion that covers a greater area
Another point to consider is the patient’s ability to tolerate the RFN procedure. In our practice, conventional RFN is 80°C, and the time it takes to create the lesion is 210 seconds for each medial branch. Comparatively, for cooled RFN, the temperature is 60°C with a total lesion time of 150 seconds for each nerve. This difference in procedure time is compounded further for multiple lesions.
Our clinic recently completed a small retrospective study of 60 patients comparing imaging times of these procedures and found that the imaging time of conventional RFN was significantly longer than that of cooled RFN.
Moreover, in 2012, a large systematic review analyzing the therapeutic effectiveness of sacroiliac (SI) joint interventions indicated better evidence for cooled RFN than conventional RFN. These results were directly attributable to the larger burn area that the cooled RFN probe generated, which could account for the variability in the SI joint nerves.
In summary, cooled RFN is as safe as conventional RFN for treating low-back pain. With better results that are directly attributable to the large burn area, along with cooled RFN’s shorter procedure times, we recommend cooled RFN for treating Selena’s lumbar facet pain.
Wenbao Wang, MD, and Jianguo Cheng, MD, PhD, respond
Selina’s case is a common one. She has chronic low-back pain, and her MRI indicates facet arthropathy. The diagnosis is further confirmed by 2 diagnostic medial branch blocks
Numerous studies and clinical trials have reported the clinical efficacy and safety of conventional RFN. In fact, conventional RFN is the standard treatment for facet mediated pain and can provide from 6 to 12 months of relief.
Many professional society guidelines recommend conventional RFN. After a comprehensive review of the literature, the American Society of Interventional Pain Physicians published its guidelines in 2013 and stated, “There is good evidence for conventional RFN for the treatment of chronic lumbar facet pain both in the short- and long-term.”
The American Association of Neurological Surgeons and the Congress of Neurological Surgeons Joint Committee published their guidelines in 2014 and stated, “There is moderate evidence that facet medial nerve neurotomy (conventional RFN) produces a short-term decrease of facet-mediated chronic low-back pain.”
Cooled RFN is used to treat pain arising from the SI joint. It is also suggested for treating thoracic (upper-back) facet joint mediated pain. Cooled RFN is thought to create a bigger lesion than conventional RFN. A larger lesion may be necessary to overcome the anatomic variations of the sacral nerves in the SI joints and the medial branches in the thoracic facet joints.
The benefits of conventional RFN
We suggest, however, that conventional RFN is the better technique in Selena’s case for the following reasons:
First, the anatomy of the medial branches in the lumbar spine is relatively consistent. If the RFN electrodes are placed accurately, the result should be predictable. With imaging guidance and sensory/motor stimulation, conventional RFN is a straightforward procedure.
Furthermore, the International Spine Intervention Society recommends that, for lumbar medial branch neurotomy to be anatomically accurate, electrodes should be placed parallel to the target nerve. The goal is not to make a larger lesion, but a more precise one.
Second, the safety of using cooled RFN for lumbar facet pain has never been evaluated. To our knowledge, not a single study of the use of cooled RFN for lumbar facet pain has been published. We, therefore, argue against using cooled RFN for lumbar facet pain. Instead, we prefer using conventional RFN to achieve precise, controlled lesions of the medial branch nerves.
In fact, conventional RFN is one of the most commonly performed procedures across the United States, with an excellent safety record. In contrast, no evidence exists to support the safety, efficacy, and cost-effectiveness of cooled RFN for lumbar facet pain. It is concerning to use cooled RF to create a large lesion in the spinal canal area, which is filled with complex neural and vascular structures.
Finally, cooled RFN is an expensive procedure. Conventional RFN for lumbar facet pain is the second most commonly performed procedure in the United States and the routine use of cooled RFN will increase health care costs.
In summary, conventional RFN is the standard of care for lumbar facet pain. It is safe, effective, and our recommendation for Selena’s treatment plan.
Keywords
Ablation: The removal of living tissue. In the case of radiofrequency ablation, it the removal of nerve tissue, which is also called “denervation.”
Arthropathy: Any disease of the joints.
Electrode: A conductor through which electricity enters or leaves an object, substance, or region.
Lesion: Any tissue damage, such as a cut, a burn, a wound. Sometimes, lesions are caused to treat a disease or condition.
Medial nerve branch: Small nerves that feed out from the facet joints in the spine and carry pain signals from the facet joints to the brain.
Nerve block: A procedure in which an anesthetic is injected near small medial nerves connected to a specific facet joint.
Spinal stenosis: A decrease the amount of space available for the nerve roots as they exit the spinal canal.